About
The Outreach Committee provides endless opportunities for students to connect with communities of various age groups from young children to adults. Organizations and institutions such as UCLA Health, Parkinson's Community Los Angeles, and St. Sebastians have partnered with the Outreach Committee in executing events for members to positively impact the common good. Furthermore, the Outreach Committee participates in health fairs, volunteers alongside clinics, creates educational materials for communities beyond UCLA campus, and executes fundraising events for a variety of charities. Outreach is dedicated to advocating for individuals with neurodegenerative diseases and providing an enriching experience in connecting to a broader audience. Above all, the Outreach Committee provides students a platform to create, educate, and inspire.
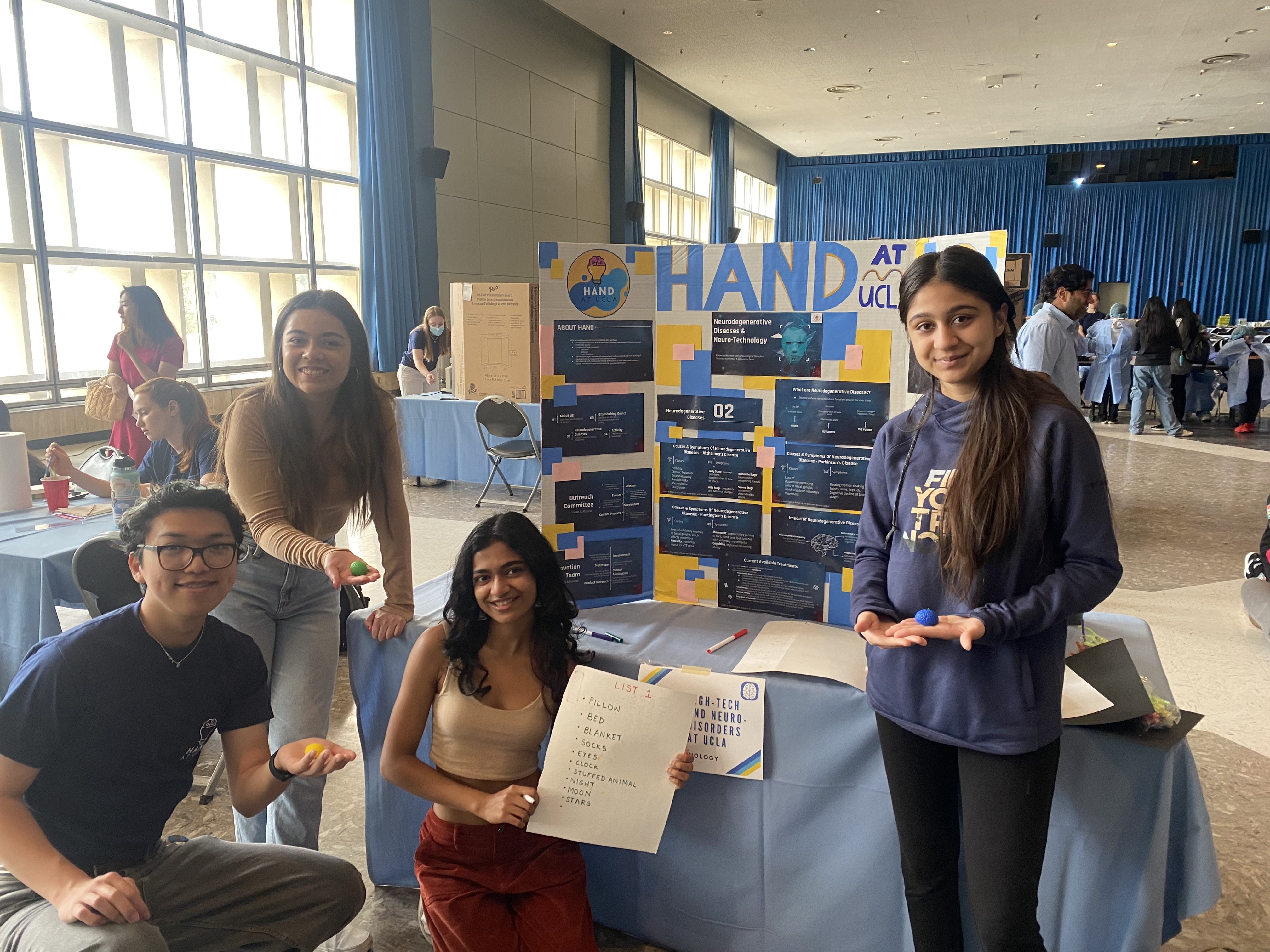
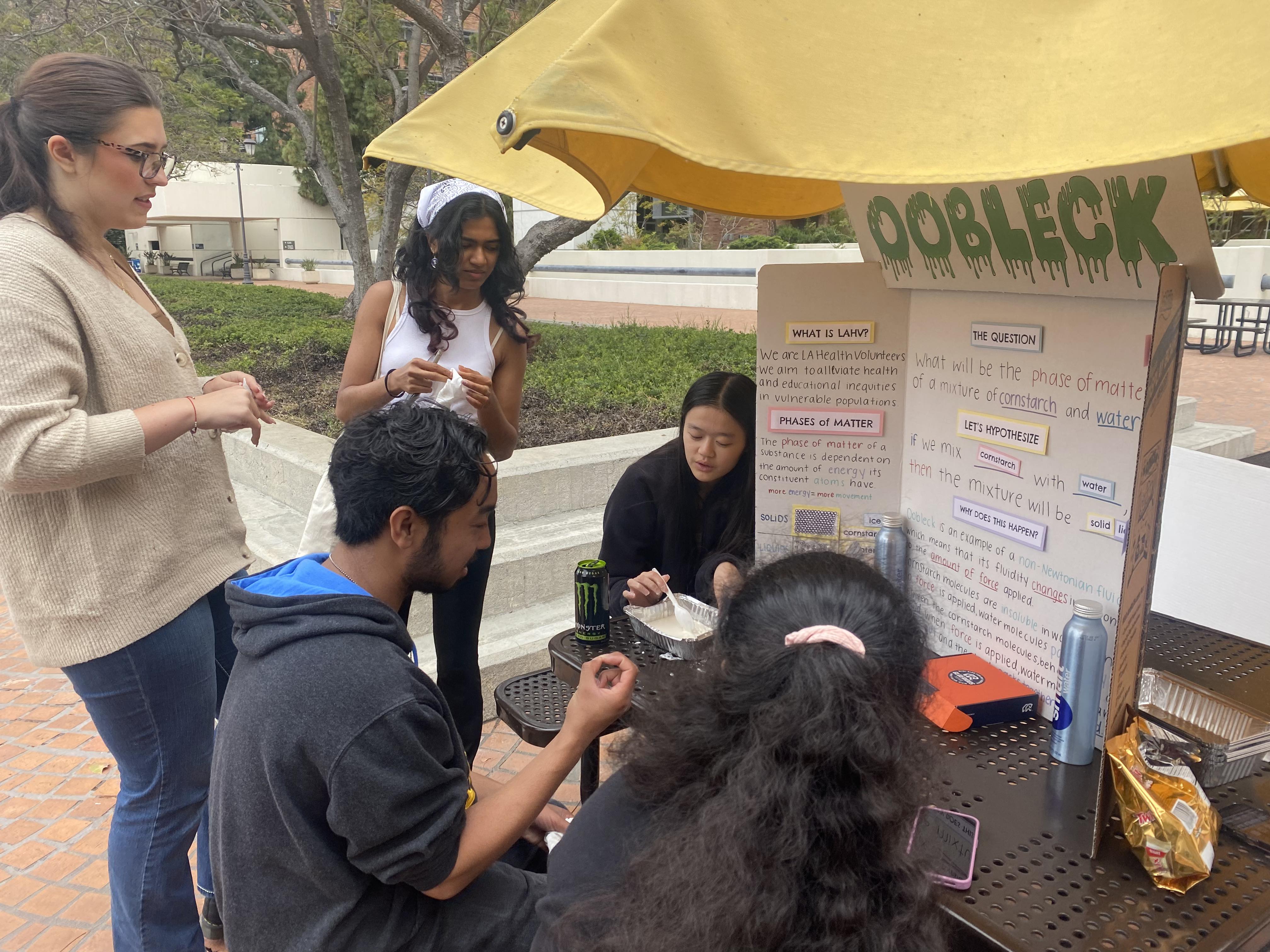
A peek at our 2022-2023 activities!
Pictured below are our Interaxon Fair presentation and the Spring Fair that we hosted!
Blogs
Click to read!
Click again to close and choose new blog post
Spinal Cord Stimulation
By Max Orr, Alex Wu, and Daniel Hong
December 6th, 2020
Spinal Cord Stimulation Overview
What is Spinal Cord Stimulation (SCS)? SCS is a means of alleviating chronic pain in patients by stimulating spinal cord nerve fibers. These electrical impulses help inhibit pain signals that are sent to the brain. This form of treatment, previously questioned by many pain specialists about its safety and efficacy, has recently begun to make a comeback in being an effective, alternative treatment after exhausting other noninvasive forms of treatment. The patient will generally have a surgically implanted device, consisting of a battery pack and electrodes, that delivers electrical impulses to the spinal nerves blocking pain signals.
With a steady growth of chronic pain patients over the years, the need for SCS has also risen. SCS has been shown to deliver therapeutic results to patients: the sympatholytic effect. More specifically, this type of effect plays a major role in downplaying the activity of the sympathetic nervous system, thus decreasing the chronic pain experienced by the patient. Generally, SCS will be offered for patients experiencing failed back surgeries, neuralgia, neuropathy, and phantom limb pain. Ultimately, SCS improves a patient’s sleep patterns, quality of life, and reduces the need for ingested pain medicines.
Spinal Cord Stimulation in Chronic Pain
Spinal cord stimulation currently serves as an intervention for chronic back and leg pain, especially should other therapies fail to adequately manage these issues on their own. Using stimulators and electrical signals, pain signals for chronic conditions can be inhibited before they are registered by the brain.
Generally speaking, applications of SCS towards chronic pain involve a neurostimulator as a power source and sets of wires and electrodes to effectively deliver electrical pulses to the stimulation site at the spinal cord. Such pulses are now adjustable in amplitude, frequency, and duration, allowing the implementation of SCS to be tailored to the specific conditions of each individual patient. Furthermore, recent developments have allowed for outputs to be more precise in location and timing, and with such tools, SCS is targeted to only inhibit the pain signals it intends to alleviate for the patient without interrupting other signals the body routinely sends.
As a field, SCS is still rapidly evolving, with research being invested into increasing battery life and reliability, or developing less invasive methods for implantation. Development of increasingly accurate sensors is also a field of investigation. However, though SCS is a promising pain relief technology with many potential applications in chronic conditions, it is currently a novel and last-resort therapy used following attempts to control pain through more traditional means. The frequency of SCS application is expected to increase as the technology matures.
Spinal Cord Stimulation in Parkinson's
For Parkinson’s patients who’ve gone through deep brain stimulation (DBS) -- one of the well-known methods of reducing Parkinson’s Disease -- and had ineffective outcomes, SCS has recently been shown to decrease pain and reduce motor symptoms. Furthermore, other drug-treatment resistant patients also reported a decrease in pain after SCS.
Spinal Cord Stimulation, as mentioned before, is an invasive treatment, meaning the treatment goes inside the body. It plants electrodes near the patients’ spines and stimulates the electrodes in either continuous, on-off bursts, or continuous bursts of varying intensities. These bursts and intensities are then programmed depending on the patient for treatment.
According to a study by Chakravarthy et al., 2020, When SCS was performed on 15 patients: 100% reported a pain reduction of an average reduction of pain being 59%. Furthermore, 73% of the patients experienced an improvement of 12% in the 10 meter walk test -- a common test to analyze the physical mobility of Parkinson's patients, while 64% of the patients experienced improvements of around 21% in the Timed Up and Go test--another test to analyze physical balance and stability.
However, as with most treatment options, SCS also has its own side effects such as jolting, infection, seroma, and hematoma. Furthermore, it should be noted that as of current, no determination has been made on whether SCS should be used as a main, on-the-side, or last ditch method of treatment; it is effective and has the potential to fit in any of the 3 categories.
References
Vannemreddy, P., & Slavin, K. (2011). Spinal cord stimulation: Current applications for treatment of chronic pain. Anesthesia: Essays and Researches, 5(1), 20. https://doi.org/10.4103/0259-1162.84174
“Spinal Cord Stimulation - About.” Medtronic, 2019, www.medtronic.com/us-en/healthcare- professionals/therapies-procedures/neurological/spinal-cord-stimulation/education-training/about-the-therapy.html.
Hegarty, Dominic. "Spinal Cord Stimulation: The Clinical Application of New Technology." Anesthesiology Research and Practice, vol. 2012, Article ID 375691, 5 pages, 2012. https://doi.org/10.1155/2012/375691
Chakravarthy, K.V., Chaturvedi, R., Agari, T. et al. Single arm prospective multicenter case series on the use of burst stimulation to improve pain and motor symptoms in Parkinson’s disease. Bioelectron Med 6, 18 (2020) https://doi.org/10.1186/s42234-020-00055-3
Gut-Brain Link
By Giorgio Conta and Justin Quan
December 6th, 2020
If you’ve ever felt butterflies in your stomach when you feel nervous, you may not know it, but these signals are coming from what some refer to as your second brain. There exists a dense network of neurons in your gut that are hidden within the walls of your digestive tract, and these neurons have a strong influence on your mood, emotions, and how you think and process your thoughts. This relatively recent discovery gives a whole new meaning to “going with your gut.” Although this network of neurons in the gut may be colloquially referred to as the second brain, scientists refer to it as the enteric nervous system (ENS), and as the years go by scientists are discovering more and more about the ENS. Based on what we know now, the ENS is composed of two thin layers lining the gastrointestinal tract, which runs from your esophagus to rectum, and comprises hundreds of millions of nerve cells. Although the brain has billions of nerve cells, scientists have determined that the ENS has a significant effect on yourself, especially concerning your emotions and mood. For this and many other reasons, scientists are finding ways in which the ENS, or at least the environment in which the ENS is housed, can be manipulated to induce positive behavioral and physiological effects. The bulk of the research on manipulation of the ENS is concerned with modulation of pain in cancer patients undergoing chemotherapy as well as determining the root cause of autism. Chemotherapy wreaks havoc on cancer patients’ digestive tract as diarrhea and anorexia are common side effects, thus researchers at Ohio State University wondered if it was possible to test the effects of microbiota manipulation on the presence of these negative side effects of chemotherapy. They believed that the microbiota manipulation would effectively change the environment of the ENS positively, such that the negative digestive side effects commonly associated with chemotherapy would diminish. They were able to test this hypothesis utilizing mice whose guts had been manipulated before chemotherapy through the administration of antibiotics and coprophagia, in which the mice eat their own and the feces of other mice. They found that the mice with altered guts that ate the poop of healthy mice not undergoing chemotherapy responded much better to the chemotherapy than the other mice, likely due to the relationship between the ENS and the mood of the mice. This principle can be applied in the future as scientists will be able to alter the diet of cancer patients as well as administer probiotics to limit the negative side effects that arise due to chemotherapy. This practice wouldn’t help the treatment of cancer itself, but it could potentially diminish the digestive problems associated with chemotherapy, thus significantly enhancing the quality of life of cancer patients undergoing chemotherapy.
While it is generally agreed that autism is a disorder in the brain, little is actually known about the root causes of Autism spectrum disorder (ASD). According to researchers at Cambridge University, there appears to be a relationship between gut health and the onset of the development of autism. To bridge the connection between neurodevelopmental disorders and “microbiotic composition,” researchers conducted a thorough review of the literature. Interestingly, researchers at Cambridge “found that abnormalities in carbohydrate digestion and absorption could explain some of the gastrointestinal problems observed in a subset of ASD patients.” Thus, it can be hypothesized that “nutrition-related factors” played a “causal role in the aetiology of ASD and its symptoms.” In their conclusion, Sande et al. highlighted promising results in “recent trials involving gluten-free diets” where the gut health and symptoms of patients were evaluated. The Cambridge study was able to conclude that environmental influences, such as nutrition, may trigger “unstable bases of a genetic predisposition which may lead to the development of autism.” A similar study on the possible role of the Microbiota-Gut-Brain-Axis to ASD was published in the International Journal of Molecular Sciences. In their study, Srikantha et al. point to a “possible link between ASD and the gut microbiota as many autistic children have co-occurring gastrointestinal problems.” Through a systematic review of the PubMed databank and online books, Srikantha et al. studied the “connection between the microbiota/microbiome and ASD.” The paper goes on to suggest that ASD is “associated with an unbalanced gut microbiota (dysbiosis).” According to Srikantha et al., this finding is particularly interesting because of the diagnostic and therapeutic value of “bacterial-derived compounds as new possible biomarkers.” Both Srikantha et al. and Sande et al. point out that the cause-effect relationship between gut microbiota and ASD is not yet well established. Thus, more data and analysis are needed to firmly establish the connection between ASD and gut health. Without a doubt, a lot remains to be learned about the mind-gut link. Jay Pasricha, M.D., director of the Johns Hopkins Center for Neurogastroenterology, suggests that the interactions between the nervous system and gut hormones and microbiota extends into higher cognition functions and other health conditions. Pasricha, however, also says that these are areas “that need more research.”
References
“The Brain-Gut Connection.” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/wellness-and-prevention/the-brain-gut-connection.
Carabotti, Marilia, et al. “The Gut-Brain Axis: Interactions between Enteric Microbiota, Central and Enteric Nervous Systems.” Annals of Gastroenterology, Hellenic Society of Gastroenterology, 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/.
Clapp, Megan, et al. “Gut Microbiota's Effect on Mental Health: The Gut-Brain Axis.” Clinics and Practice, PAGEPress Scientific Publications, Pavia, Italy, 15 Sept. 2017, www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/.
“The Gut-Brain Connection.” Harvard Health, www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection.
Marijke M. H. van De Sande, et al. “Autism and Nutrition: the Role of the Gut–Brain Axis: Nutrition Research Reviews.” Cambridge Core, Cambridge University Press, 8 July 2014, www.cambridge.org/core/journals/nutrition-research-reviews/article/autism-and-nutrition-the-role-of-the-gutbrain-axis/76735D9541EB3D2A86099583F42B39CF.
Miller, Rachel. “The Gut Brain Connection: Does Our Diet Affect Our Mood?” Knowledge Box, kb.gcsu.edu/src/2020/oral_presentations/27/.
Srikantha, Piranavie, and M. Hasan Mohajeri. “The Possible Role of the Microbiota-Gut-Brain-Axis in Autism Spectrum Disorder.” MDPI, Multidisciplinary Digital Publishing Institute, 29 Apr. 2019, www.mdpi.com/1422-0067/20/9/2115.